Organ Transplant
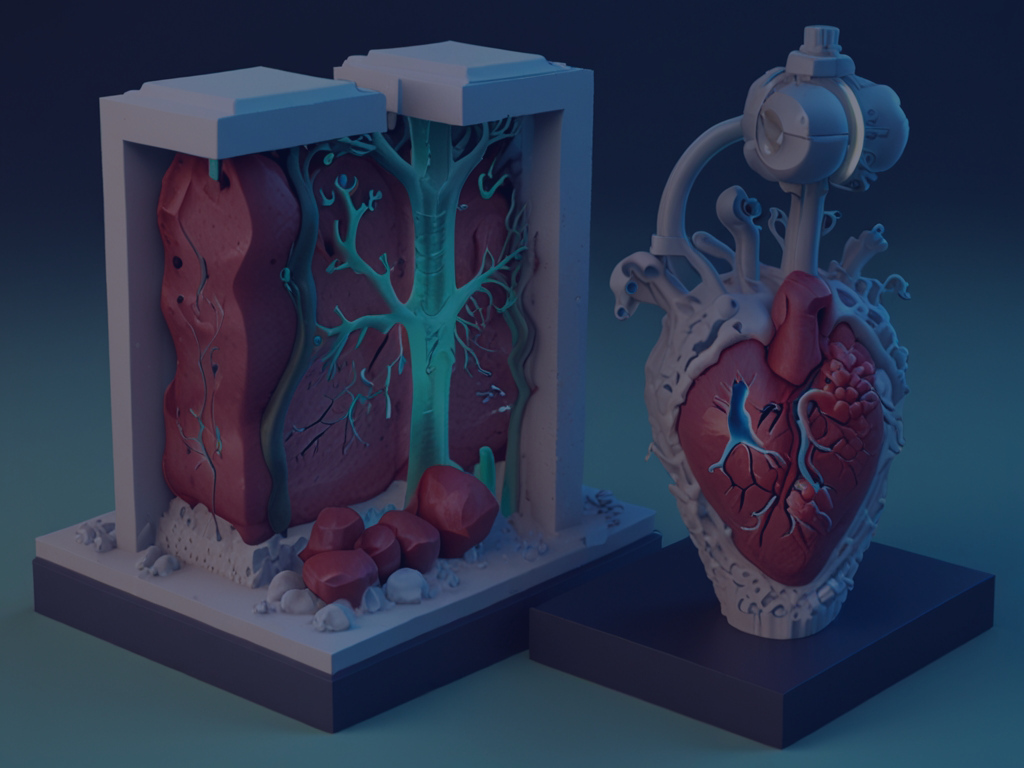
Organ transplant is a medical procedure in which a failing or damaged organ in a patient’s body is
replaced with a healthy organ from a donor. This treatment is used to replace organs such as the heart, kidneys, liver, lungs, pancreas, or intestines when they are no longer functioning properly due
to disease, injury, or congenital conditions.
Key points about organ transplants:
1. Types of Organ Transplants:
- Living Donor Transplants: A healthy person donates part of an organ, such as a
kidney or liver, to a recipient. - Deceased Donor Transplants: Organs are donated by individuals who have died,
often after brain death, and are recovered for transplant. - Autografts: Tissue or organs transplanted from one part of the patient’s body to
another. - Allografts: Organs or tissues transplanted between individuals of the same species
2. Matching and Compatibility:
- Organs from a donor must be compatible with the recipient’s body to reduce the risk
of organ rejection. This involves matching blood types, tissue markers (HLA), and
other factors. - Immunosuppressive drugs are used to prevent the body from rejecting the
transplanted organ by suppressing the immune system.
3. Donor and Recipient Considerations:
- The availability of donor organs is a major issue. Thousands of people are on
transplant waiting lists, but not all will receive an organ in time. - Ethical issues can arise around organ donation, such as consent, allocation, and the
use of organs from living or deceased donors.
4. Risks and Challenges:
- Rejection: The body may recognize the transplanted organ as foreign and attempt to
destroy it. This is why lifelong monitoring and medication are often necessary. - Infection: Immunosuppressive drugs can increase the risk of infections.
- Organ Failure: The transplanted organ can sometimes fail due to complications or
rejection.
5. Outcomes:
The success rate of organ transplants has improved significantly due to advances in
surgical techniques, immunosuppressive medications, and post-operative care.
However, success varies depending on the organ and the individual’s health.
6. Global Organ Shortage:
There is a critical shortage of donor organs worldwide, leading to long waiting times
for many patients. Efforts to address the shortage include increasing awareness of
organ donation, improving organ preservation techniques, and exploring alternatives
like bioengineering or xenotransplantation (transplanting organs from animals)
7. REGULATION OF MEDICAL PRACTITIONERS
8. As per Section 3(4) of the Act, only a registered medical practitioner can
remove an organ from a human body and the registered medical
practitioner can conduct transplantation only in a hospital registered under
the Act. A medical practitioner does not need a separate registration under
the Act. Section 2(n) of the Act defines a “registered medical practitioner” to
mean a medical practitioner who possesses any recognized medical
qualification as defined in clause (h) of Section 2 of the Indian Medical
Council Act, 1956 (5) and who is enrolled on a State Medical Register as
defined in clause (k) of that section. The Act prescribes various duties of a
medical practitioner and also punishment for breach of those duties.
9. In case of cadaver donation, the registered medical practitioner has to
satisfy himself that the donor has been certified as brain-stem dead as
described above.
10. When potential cadaver donor is <18 years of age, any of the parents of the
deceased person may give authority for the removal of any human organ
from the body of the deceased person.
11. In case of living donation, the registered medical practitioner has to explain
all possible effects, complications, and hazards connected with the removal
and transplantation to the donor and recipient, respectively, before
undertaking the removal or transplantation of any human organ.
12. PUNISHMENT UNDER THE ACT
As per Section 18 of the Act, any person involved in removal of any human
organs without authority can be punished with imprisonment for a term
which may extend to 10 years and with fine which may extend to Rs. 20
lakhs. If that person is a registered medical practitioner who is convicted,
his name shall be reported by the Appropriate Authority to the respective
State Medical Council for taking necessary action including removal of his
name from the register of the Council for a period of 3 years for the first
offense and permanently for the subsequent offense.
14. As per Section 19 of the Act, any person involved in commercial dealing in
human organs can be punished with imprisonment for a term which shall
be not less than 5 years but which may extend to 10 years and shall be
liable to fine which shall not be less than Rs. 20 lakhs but may extend to Rs.
1 crore.
15. As per Section 20 of the Act, any person who contravenes any other
provision of the Act can be punished with imprisonment for a term which
may extend to 5 years or with fine which may extend to Rs. 20 lakhs.
16. It is unfortunate that when anything goes wrong with the legal aspects of
transplant, it is the doctors who are considered responsible. In July 2016, a
kidney transplant was stopped midway when it was realized that an
unrelated donor transplant was being performed as related donor transplant. The police arrested doctors of the transplant team, medical
director, and CEO of the hospital using TOHA sections 12 (‘no registered
medical practitioner shall undertake the removal or transplantation of any
human organ unless he has explained, in such manner as may be
prescribed, all possible effects, complications, and hazards connected with
the removal and transplantation to the donor and the recipient,
respectively’) and section 21 (‘The Act has been committed by a company
and it is proved that the offense has been committed with the consent or
connivance of, or is attributable to any neglect on the part of, any director,
manager, secretary, or other officer of the company. Such director, manager,
secretary, or other officer shall also be deemed to be guilty of that offense
and shall be liable to be proceeded against and punished accordingly’).[8
]
17. The authors wonder that when there is an elaborate process to obtain
approval for transplant why are the doctors made liable? There is a hospital
committee (and in case of unrelated transplant a state committee also)
meant to verify all the documents submitted by the recipient and donor to
establish the identity and relationship between recipient and donor. Then
the recipient, the donor, and their relatives are interviewed by these
committees. The whole process is video recorded. If there is such an
extensive process, why are transplant doctors made responsible? Moreover,
should the doctor be verifying the documents or concentrating in
management of the patient?
18. In summary, Transplantation of Human Organs Act, 1994, was a significant
advance in the field of organ transplant in India. Most importantly, it
legalized brain-stem death, making cadaver donor transplant possible. The
Act has significantly regulated living donor transplant but made the process
of obtaining approval difficult even in genuine cases. Punishment is harsh
for anyone who contravenes any provision of the Act and unfortunately,
transplant team doctors are made liable in most cases.

